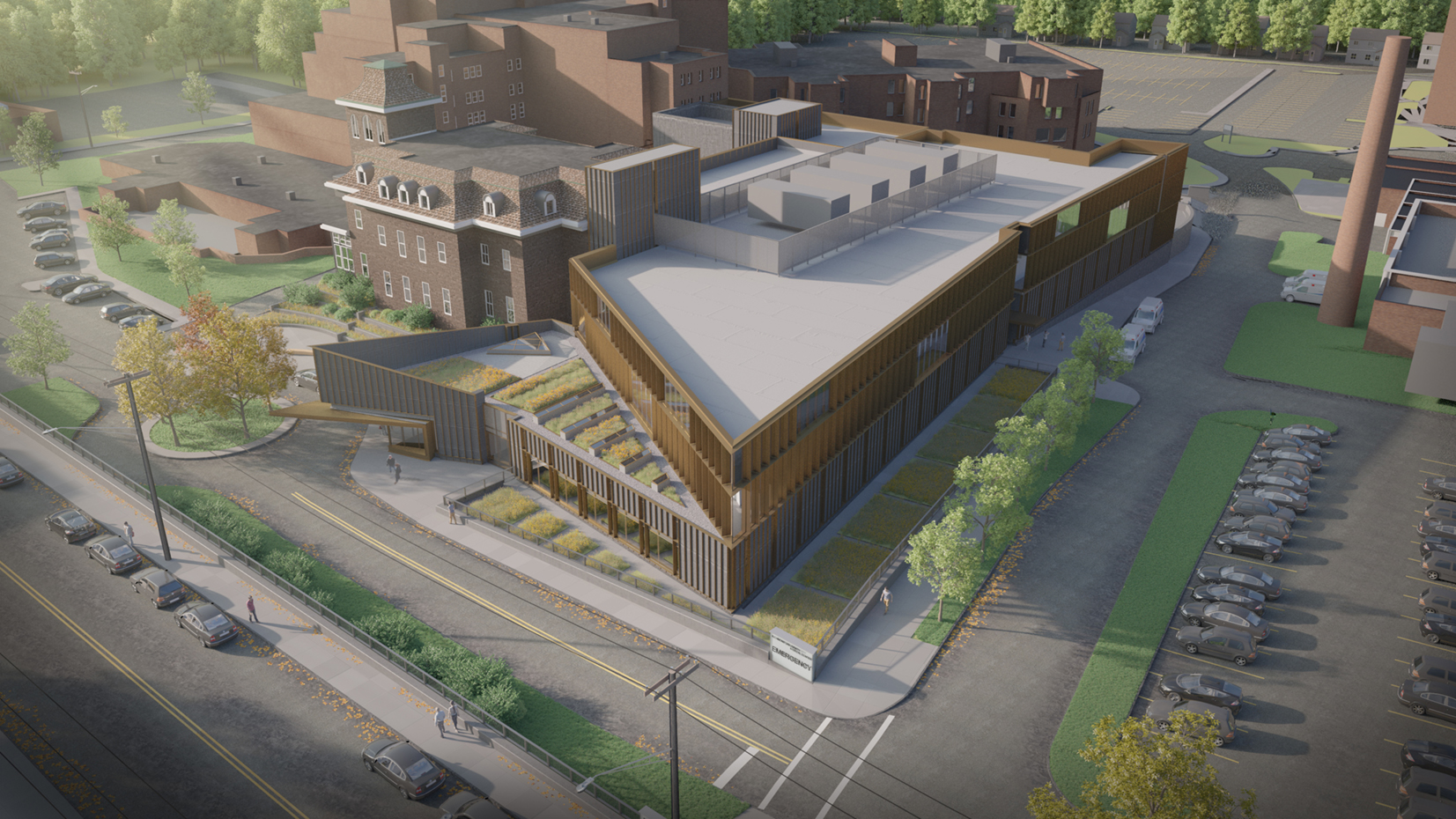
An emergency department designed with resiliency in mind
To meet the increasing healthcare demands of Staten Island’s fastest growing communities and remain resilient from potential natural disasters, Richmond University Medical Center (RUMC) needed to replace its outdated emergency department (ED). The existing facility was built to accommodate 25,000 patients annually, however, current patient volumes at RUMC have increased significantly to nearly 70,000 per year. Learning from the aftermath of Hurricane Sandy–where the ED treated five times its normal patient volume–RUMC sought a design solution that would better equip its Level 1 Trauma Center in the future. The new ED, set to open in 2018, is designed to optimize the patient experience through connectivity to other treatment areas combined with a planning approach that allows for future campus expansion.
The new and expanded ED will include centers for trauma, urgent care, pediatrics and other specializations while encompassing 51 treatment spaces and a 12-bed observation unit. The design solution also introduces a dual-track ED model that filters the patient volume into acute-care and lower-acuity areas to improve the overall flow of patients, visitors and staff in the ED.
The new design provides RUMC the ability to provide more focused care and realize operational efficiencies, flexibility and adaptability, and future synergies for strategic campus master planning. The ED is strategically located to connect with the hospital’s existing hospital radiology department and other key program adjacencies, minimizing travel distances and limiting disruption to patients. It also allows for additional clinical services along with expansion of ORs and ICUs to be added in future phases.